Background: Marginal zone lymphomas (MZLs) are a heterogenous group of indolent non-Hodgkin lymphomas that include extranodal MZL of mucosa-associated lymphoid tissue (EMZL or MALT lymphoma), nodal MZL (NMZL), and splenic (SMZL). All three subtypes can transform to diffuse large B-cell lymphoma (DLBCL). However, the cumulative incidence of histologic transformation (HT) and survival of patients with transformed MZL (t-MZL) in the US population have not been reported to date. Hence, we sought to estimate the risk of HT and relative survival (RS) in patients diagnosed with MZL in USA using a population-based study.
Method: We conducted a population-based cohort study of t-MZL using the Surveillance, Epidemiology, and End Results-17 database. We included adults diagnosed with MZL in the US between 2011-2015. This time period was selected to provide a contemporary estimate of survival and allow for adequate follow-up. We identified patients with t-MZL by following patients with MZL and identifying those patients with subsequent diagnoses of DLBCL. All patients with t-MZL had biopsy-proven HT. We estimated the post-transformation RS of patients with t-MZL using flexible parametric survival models with 5 degrees of freedom for the baseline cumulative hazard. We compared the survival of the different MZL subtypes using multivariable modeling after adjusting for age, year, race, Ann Arbor stage, B symptoms, and geographic location. P values less than 0.05 were considered statistically significant.
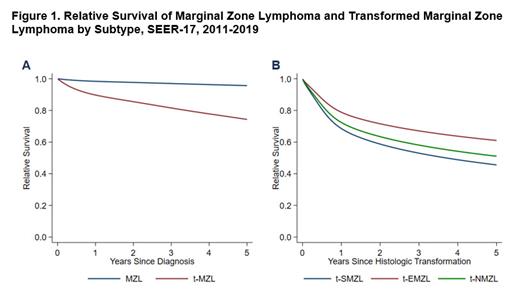
Results: A total of 5372 patients with MZL were included in the study. There were 3446 (64.2%) patients with EMZL, 1485 (27.6%) with NMZL, and 441 with SMZL (8.2%). Among the 5372 patients, 121 (2.3%) had biopsy-proven HT after a median follow-up of 6.2 years (95% confidence interval (CI), 6.1-6.3). HT was associated with decreased survival for patients with MZL ( Figure 1A). Among the MZL subtypes, SMZL was the most likely to develop HT (24/441, 5.4%), followed by NMZL (49/1436, 3.3%) and EMZL (48/3398, 1.4%) ( P < 0.001) despite similar follow-up between groups. The 5-year post-transformation RS was highest for t-EMZL (61%) followed by t-NMZL (51%) and t-SMZL (46%) (Figure 1B). On multivariable analysis, however, the subtype of MZL was not a significant predictor of RS. In addition, there were no significant predictors of RS identified among the study covariates.
Conclusion: This is the first population-based study to date reporting outcomes associated with t-MZL in the USA. The risk of HT in MZL may vary depending on the subtype of MZL with cumulative incidence of 1.4-5.4% observed after 6 years of follow-up in the contemporary era. HT was associated with increased mortality irrespective of MZL subtype. Among the MZL subtypes, SMZL was most likely to develop HT and had the lowest estimated 5-year RS. Additional studies are needed to better understand factors associated with prognosis in t-MZL.
Disclosures
Epperla:Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Incyte: Speakers Bureau; Beigene: Research Funding, Speakers Bureau; ADC Therapeutics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Lilly: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal